|
 |
| [ Ana Sayfa | Editörler | Danışma Kurulu | Dergi Hakkında | İçindekiler | Arşiv | Yayın Arama | Yazarlara Bilgi | E-Posta ] | |
| Fırat Tıp Dergisi | |||
| 2009, Cilt 14, Sayı 4, Sayfa(lar) 290-292 | |||
| [ Özet ] [ PDF ] [ Benzer Makaleler ] [ Yazara E-Posta ] [ Editöre E-Posta ] | |||
| Cerebellitis due to Antituberculosis Therapy in a Patient with Chronic Renal Failure | |||
| Meliha TAN1, Özlem ALKAN2, Sibel KARACA1, Başak KARAKURUM GÖKSEL1, Yusuf Ziya DEMİROĞLU3 | |||
| 1Başkent Üniversitesi Tıp Fakültesi, Nöroloji Anabilim Dalı, ADANA, Türkiye 2Başkent Üniversitesi Tıp Fakültesi, Radyoloji Anabilim Dalı, ADANA, Türkiye 3Başkent Üniversitesi Tıp Fakültesi, İnfeksiyon Hastalıkları Anabilim Dalı, ADANA, Türkiye |
|||
| Keywords: Chronic renal failure, isoniazid, cerebellitis, Magnetic Resonance Imaging, Kronik renal yetmezlik, izoniazid, serebellit, Manyetik Rezonans Görüntüleme | |||
| Summary | |||
The incidence of tuberculosis in patients treated with hemodialysis for chronic renal failure is higher than in the general population. Further, those
patients often experience adverse effects from therapy with anti-tuberculosis drugs. Although the ototoxicity and toxic retinopathy caused by antituberculosis
drugs is well known, the cerebellar syndrome is rare. We presented a 50-year-old woman developed cerebellar ataxia who was on
hemodialysis program and taking anti-tuberculosis drugs combination therapy. Brain magnetic resonance imaging showed cerebellar edema.
Cerebellar signs partially reversed after discontinuation of anti-tuberculosis therapy and initiation of pyridoxine therapy. In our patient, isoniazid was
probably the drug that caused cerebellar signs and symptoms. In conclusion, a diagnosis of isoniazid-induced cerebellitis should be considered when
cerebellar signs develop in patients undergoing hemodialysis and treated with isoniazid. |
|||
| Introduction | |||
The incidence of tuberculosis (TB) in patients with chronic
renal failure (CRF) is reported to be 10-fold greater than that
in the general population, possibly because of decreased
cellular immunity in those patients1,2. The treatment of
TB in patients with CRF may be complicated by an increased
risk of toxicity from anti-tuberculosis drugs. Ototoxicity,
optic neuritis, and central and/or peripheral neurotoxic effects
are well-known adverse effects of treatment with
streptomycin, ethambutol, and isoniazid (INH)3. However,
there are rare reports of cerebellar syndrome caused by antituberculosis
drugs1,4,5. We presented a patient with CRF
whose cerebellar ataxia was caused by anti-tuberculosis drug
therapy and the probable role of INH in cerebellar
inflammation was discussed. |
|||
| Case Presentation | |||
A 50-year-old woman with CRF caused by hypertensive nephropathy had been undergoing hemodialysis 3 times per
week for 10 months. She complained of fever and
moderate malaise of 1 month’s duration. In general
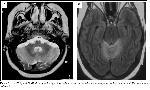
examination there were palpable cervical lymph nodes. Cmputerized tomography (CT) of neck revealed some cervical lymph nodes enlargement. The results of cervical lymph node biopsy indicated tuberculosis lymphadenitis. Thorax CT was normal. The patient was treated with a combination of 5 antituberculosis drugs: pyrazinamide 2500 mg/d, INH 300 mg/d, rifampicin 600 mg/d, and ethambutol 1500 mg/d administered 3 times per week after each hemodialysis treatment, and streptomycin 1g 3 times per week administered 6 to 8 hours before each hemodialysis treatment. Because she experienced hearing and visual loss 2 weeks after the initiation of anti-tuberculosis treatment, therapy with ethambutol and streptomycin was terminated. At that stage, the MR imaging showed no abnormality in the cerebellum and hepatic function tests (aspartat and alanin transaminase) were in normal ranges. Therapy was continued with INH, rifampicin, and pyrazinamide. Two months later, she exhibited a mild intentional tremor and severe truncal ataxia, and she could not stand, sit, or walk without help. The results of motor and sensorial examinations were within normal limits, and no pathologic reflexes were noted. Results of the patient’s cerebrospinal fluid (CSF) analysis revealed a mild elevated protein and a glucose level within the normal range. The results of testing for infectious diseases and cultures of the CSF were also within normal limits. Brain MR imaging showed diffuse cortical hyperintensity in both cerebellar hemispheres and vermis (Figure 1a, b). Anti-tuberculosis therapy was terminated, and treatment with pyridoxine 100 mg/d was initiated. Five months after discharge, a neurologic examination revealed mild ataxia with hearing and visual disturbance. In the follow-up brain MR examinations, cerebellar hyperintensity was persisting on the FLAIR and T2-weighted images.
|
|||
| Discussion | |||
A high incidence of side-effects associated with antituberculosis
drug treatment in patients with CRF has been
reported. As the incidence of TB is increased in these
patients, it is expected to encounter side effects of antituberculosis
drugs more frequently in this patient
population. Moreover, renal failure can increase the
tendency to the occurrence of side effects of drugs. The
neurotoxic effects of INH are well known, ranging from
peripheral neuropathy, encephalopathy, and seizure to
psychiatric disorders1-5. In the literature, only a few of
hemodialysis patient was reported to suffer from INH
induced cerebellar syndrome1,4,5. Blumberg and Gil
published a report of reversible INH -associated cerebellar
dysfunction in a patient with CRF. In that case, cerebellar
toxicity was completely reversed after giving pyridoxine
and reducing the INH dosage5. Siskind et al described
ataxia caused by INH toxicity in 2 patients with end-stage
renal disease1. Those authors observed that INH
toxicity tended to occur in patients receiving pyridoxine
supplements of less than 100 mg/d, and they recommended
100 mg/d of pyridoxine supplementation for hemodialysistreated
patients who require INH. However, Cheung et al
reported 3 hemodialysis-treated patients in whom INH -
induced encephalopathy developed despite prophylactic
pyridoxine4. While the beneficial effect of pyridoxine
on peripheral neuritis has been established, its role in
prevention or treatment of INH induced encephalopathy is
less certain4. In our patient, cerebellar signs partially
reversed after the discontinuation of treatment with INH,
pyrazinamide, and rifampicin and the initiation of
pyridoxine therapy. Although It was well known hepatotoxicity of INH, pyrazinamide and riphampicine, only INH was reported related to neurotoxicity6. For this reason, the cerebellar signs of presented patient must be depended on INH. Isoniazid induces neurotoxicity by inhibiting the phosphorylation of pyridoxine, which results in the decreased production of pyridoxal-5-phosphate, a coenzyme involved in multiple metabolic functions including neurotransmission via gamma-aminobutyric acid (GABA)7. Because GABA is the primary inhibitory neurotransmitter produced by cerebellar Purkinje cells, it may be important in patients with cerebellar signs caused by INH toxicity5. It is likely that the increased incidence of INH toxicity in dialysis patients is multifactorial. In these patients, INH toxicity is attributed to malnutrition, pyridoxine deficiency, a reduced degradation rate resulting from slow acetylation, and poor renal clearance of INH5. Our patient was well nourished, but her acetylation status was unknown. Drug- induced cerebellitis is primarily a clinical diagnosis made by the exclusion of other metabolic or infective causes. The close temporal relationship between the onset of cerebellar findings and the initiation of drug therapy and resolution of symptoms after stopping the drug provide strong support for such a diagnosis4. Differentiating cerebellar edema caused by drug toxicity from acute cerebellitis is difficult in MR studies. Acute cerebellitis occur as a primary infectious, post-infectious or post-vaccination disorder and mostly presents in early childhood. The most common MR imaging findings in patients with acute cerebellitis are diffuse cerebellar grayand- white matter hyperintense signals on T2-weighted images. The CSF examination may be normal or reveal pleocytosis. Clinical improvement generally precedes that demonstrated on MR imaging. Considerable clinical improvement is shown in the course of time, whereas the MR findings persist. Cerebellar atrophy is seen in the chronic phase of the disease8. Because our 50-year-old patient’s clinical findings gradually diminished after the administration of pyridoxine and the discontinuation of isoniasid, her cerebellar signs were attributed to treatment with INH. In conclusion, a diagnosis of isoniazid -induced cerebellit should be considered when cerebellar signs develop in patients undergoing hemodialysis and treatment with INH. The recognition of that disorder is important because complete or partial recovery is possible after discontinuation of anti-tuberculosis therapy and initiation of pyridoxine therapy. |
|||
| References | |||
1) Siskind MS, Thienemann D, Kirlin L. Isoniazid-induced
neurotoxicity in chronic dialysis patients: report of three cases
and a review of the literature. Nephron 1993;64:303-306.
2) Quantrill SJ, Woodhead MA, Bell CE, Hardy CC, Hutchison
AJ, Gokal R.Side-effects of antituberculosis drug treatment in
patients with chronic renal failure. Eur Respir J 2002; 20:440-
3) Hussein MM, Mooij JM, Roujouleh H. Tuberculosis and
chronic renal disease. Semin Dial 2003; 16:38-44.
4) Cheung WC, Lo CY, Lo WK, Ip M, Cheng IK. Isoniazid
induced encephalopathy in dialysis patients. Tuber Lung Dis
1993; 74:136-139.
5) Blumberg EA, Gil RA. Cerebellar syndrome caused by
isoniazid. DICP 1990;24:829-831.
6) Tostmann A, Boeree MJ, Aarnoutse RE, et al.
Antituberculosis drug-induced hepatotoxicity: concise up-todate
review. J Gastroenterol Hepatol. 2008 ;23:192-202.
|
|||
| [ Başa Dön ] [ Özet ] [ PDF ] [ Benzer Makaleler ] [ Yazara E-Posta ] [ Editöre E-Posta ] | |||
| [ Ana Sayfa | Editörler | Danışma Kurulu | Dergi Hakkında | İçindekiler | Arşiv | Yayın Arama | Yazarlara Bilgi | E-Posta ] |