While the ages of 110 participants included in the study ranged from 27 to 75, their duration of study ranged from 5 to 16 years. Patient and control groups had similar characteristics in terms of gender, marital status, level of income, existence of additional medical diseases, smoking, existence of history of suicide attempts, and substance abuse. The groups were not similar in terms of age and duration of study, and var-ied in terms of occupational groups, existence of alco-hol use, and existence of psychiatric disorder (Table
1).
Mean age of the patient group was 54. Patients were divided into two groups based on such value as <54 age and ≥54 age. Mean RLSSS scores of the two groups were 28,34±8,08 and 32,50±6,27, respectively. Groups were significantly different from one another in terms of RLSSS scores (p <0,05).
78,7% (n :37) of the patient group was female, and 21,3% (n :10) was male. While mean RLSSS score in the female group was 31,13±6,28, it was 28,00±10,79 in the male group. RLSSS scores were similar among the genders (p >0,05).
Total mean PSQI score in the female patient group 10,56±3,98, and 9,50±4,71 in the male patient group. There was no significant difference among the total PSQI scores of the patient group by gender (p >0,05).
38,3% (n :18) of the patient group was smokers, and 61,7% (n :29) was not regular smokers. While mean RLSSS scores of the smoker group was 32,11±5,56, it was 29,44±8,33 in the nonsmoker group. No signifi-cant difference was observed among the smokers and nonsmokers in terms of RLSSS scores (p <0,05). While the mean PSQI score of smokers was 12,83±3,74, the mean PSQI score of the nonsmokers was 8,79±3,58. There was significant difference among the groups (p <0,05).
Groups were compared in terms of RLSSS, WHOQOL-BREF-TR, PSQI index scores. Total RLSSS score manifested significant difference in the patient and control groups (p <0,001). WHOQOL-BREF-TR general quality of life, health satisfaction, and physical health sub-domain scores were identified as significantly higher in the control group (p <0,05). WHOQOL-BREF-TR psychological health, environ-mental health, and social relationships sub-domain scores were similar among the groups (p >0,05). Total score of PSQI index and all subdomain scores were significantly higher in the patient group (p <0,05) (Table 2).
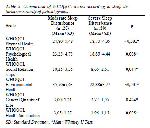
Analyzing the relationship between RLSSS and PSQI in terms of direction and level of correlation among the scales in the patient group; significant correlation in the positive direction was identified among the RLSSS and PSQI total score, subjective sleep quality, and sleep disorder sub-domains (Table 3). Analyzing the rela-tionship between RLSSS and WHOQO

Click Here to Zoom |
Table 3: Evaluation of correlations of scale scores in the patient groups. |
L-BREF-TR; there was significant correlation in the negative direction among the RLSSS, WHOQOL-BREF-TR physical health, psychological health, gen-eral quality of life, and health satisfaction sub-domains (Table 3). Analyzing the relationship between PSQI and WHOQOL-BREF-TR; there was significant correlation in the negative direction among the subjective sleep quality and social relationships. No significant correlation was observed among sleep latency and WHOQOL-BREF-TR. Weve observed significant correlation in the negative direction among all sub-domains of WHOQOL-BREF-TR except for shortened sleep duration and general quality of life. There was significant correlation in the negative direction among sleep efficiency and environmental health. There was significant correlation in the negative direction among all subdomains of WHOQOL-BREF-TR except for sleep disorder and general quality of life. There was significant correlation in the negative direction among the sub-domains of daytime dysfunction and physical health, environmental health, general quality of life, and health satisfaction. There was significant correla-tion in the negative direction among all subdomains of WHOQOL-BREF-TR except for total PSQI score and general quality of life (Table 3).
When the RLS severity of the patient population was grouped by RLSSS score, 10,6% (n :5) of the patient group had moderate, 31,9% (n :15) had severe, and 57,4% (n :27) had very severe RLS severity levels. Analyzing the relationship between the RLS severity groups and WHOQOL-BREF-TR; significant difference was identified among the groups in terms of phys-ical health and health satisfaction sub-domain scores (Table 4).

Click Here to Zoom |
Table 4: Comparison of WHOQOL and PSQI scores according to RLS (Restless legs syndrome) stages. |
Analyzing the relationship between RLS severity groups and PSQI; weve observed significant differ-ence among sleep disorder sub-domain and RLS groups (p <0,05, H :8,405), however, the differences among other sub-domains and RLS groups were not at a significant level (Table 4). Patients were grouped in terms of sleep disorder severities by total PSQI scores. Patients with score PSQI<5 were evaluated as having mild, PSQI≥5 to <10 as moderate, and PSQI≥10 as severe sleep disorder. Accordingly, 42,6% (n :20) of the patients had moderate, and 57,4% (n :27) had se-vere sleep disorder. Analyzing the relationship between the severity of sleep disorder and WHOQOL-BREF-TR; patients with severe sleep disorder had poorer quality of life compared to patients with moderate sleep disorder. Such difference was at a statistically significant degree in all domains except for general quality of life (Table 5).
Click Here to Zoom |
Table 5: Comparison of WHOQOL scores according to sleep dis-turbance severity of patient groups. |



