|
 |
| [ Ana Sayfa | Editörler | Danışma Kurulu | Dergi Hakkında | İçindekiler | Arşiv | Yayın Arama | Yazarlara Bilgi | E-Posta ] | |
| Fırat Tıp Dergisi | |||||||||||||||
| 2010, Cilt 15, Sayı 4, Sayfa(lar) 188-193 | |||||||||||||||
| [ Özet ] [ PDF ] [ Benzer Makaleler ] [ Yazara E-Posta ] [ Editöre E-Posta ] | |||||||||||||||
| Assesment of Criteria in Differentiation of Ureteral Stones from Phleboliths with Thin-Slice Unenhanced Computed Tomography | |||||||||||||||
| Koray AKDAMAR1, Mehmet Ruhi ONUR2, Çağatay ANDİÇ3, Metin ÇUBUK4 | |||||||||||||||
| 1Özel Muğla Hastanesi, Radyoloji, MUĞLA, Türkiye 2Fırat Üniversitesi Tıp Fakültesi, Radyoloji, ELAZIĞ, Türkiye 3Başkent Üniversitesi Tıp Fakültesi, Radyoloji, ADANA, Türkiye 4Akdeniz Üniversitesi Tıp Fakültesi, Radyoloji, ANTALYA, Türkiye |
|||||||||||||||
| Keywords: Computed tomography, ureteral stone, phlebolith, Bilgisayarlı tomografi, üreter taşı, flebolit | |||||||||||||||
| Summary | |||||||||||||||
Objective: The purpose of this study was to asses the accuracy of criteria in distinguishing distal urinary stones from phleboliths defined in the literature with thin-slice unenhanced helical computed tomography (CT). Materials and Methods: Between October 2004 and April 2005, we performed 3 cm length thin-slice (2 mm section thickness, pitch:1) helical CT on 31 patients with urinary stones and on 43 patients with 80 phleboliths. The size, shape, central lucency, soft tissue rim sign, comet-tail sign, density values and profile analysis of each calcification were recorded. Results: Fifty two (65%) of 80 phleboliths were round and 28 (35%) were oval shape. On the contrary, ten (32%) of 31 stone were round, 8 (26%) of them were of oval shape. Geometric configuration was seen in thirteen (42%) stones but not in any phleboliths. Mean densities of phleboliths and stones were 386,5 HU (131 HU/935 HU) and 1088 HU (526 - 1594), respectively. This difference was statistically significant (p<0,05). Eighteen (23%) of 80 phleboliths had central lucency and bifid peak on profile analysis. All 31 stones had a single peak at profile analysis. Although comet-tail sign was seen at 12 (15%) of 80 phleboliths, we did not observe this sign at stones. We observed soft tissue rim sign on 21 (67%) of 31 stones. However this sign was never seen on phleboliths. Conclusion: The results of this study indicate that unenhanced helical CT has reliable findings in the differentiation of stones from phleboliths. It is easier to differentiate urinary stones from phleboliths with thin-slice CT. Applying of all criteria mentioned in this study may be useful in differentiation of distal urinary stones from phleboliths on unenhanced helical CT. |
|||||||||||||||
| Introduction | |||||||||||||||
Urinary stones are common urological problems affecting up to 3-5% of the entire population in industrialized countries1. A diagnosis of ureteral stone disease may not be readily apparent on the basis of history, physical examination, and laboratory studies. In the past many patients with acute flank pain therefore did undergo excretory urography or sonography to determine the presence of urinary stone. Unenhanced helical CT is the technique of choice for the examination of patients with acute flank pain and suspected ureteral obstruction since this imaging modality is more effective in the detection of ureteral stones and may also reveal unsuspected pathology in the abdomen and pelvis responsible for the patient's symptoms2. However, a potential pitfall of this technique is the lack of differentiation of a distal ureteral stone from other pelvic calcifications in some cases. The most common and potentially troublesome calcification that can be confused with a ureteral stone is pelvic phlebolith3. In this study, we assesed several unenhanced CT criteria defined in literature for distinguishing distal ureteral stones from pelvic phleboliths and tried to obtain most useful ones. |
|||||||||||||||
| Methods | |||||||||||||||
Between October 2004 and April 2005, 52 consecutive patients (age range, 24-70 years) with acute flank pain referred to our clinic for unenhanced helical CT. Unenhanced helical CT revealed urinary stone in 40 of these 52 patients. However 31 patients (21 men, 10 women) were included into the study which were proven to have urinary stone by stone passage history, lithotripsy and urinary stone extracting. We performed second helical CT on these patients which was focused on stone and with thin slice. Before all CT examinations, we had scout views with 40 cm length, including abdomen and pelvis. Scout view parameters were 250 mA and 120 kV. The window level and window width were 130 and 40, respectively. Helical images were performed with focusing stone on scout image. If stone was not seen on scout image, helical imaging was performed with the aid of KUB film or intravenous urography. The length of helical image was 3 cm. CT was performed with 120 kV, 200 mA, 2 mm/rotation and 2 mm section thickness (pitch: 1). Informations acquired with helical imaging were reconstructed with 2 mm interval. Analysis of digital images were performed on workstation. Pelvic phlebolith group included patients who had abdominal CT for other reasons and evaluated with symptoms related to other system disorders, Forty three patients (25 men, 18 women) were included in this group. In these 43 patients, 80 phleboliths located along the expected course of the pelvic ureter were identified and included in this analysis. We performed 3 cm length helical CT on these patients with the same parameters as stone group. CT examinations were performed with focusing on calcification detected on scout view and abdominal CT. All CT examinations were performed with Toshiba X-Vision CT scanner. An institutional review board and ethics committee approval, and informed consent from each patient was obtained. After performing CT examinations, shape (round, oval, geometric), presence of central lucency, soft tissue rim sign (circumferential edema of the ureteral wall surrounding a calculus) and comet-tail sign (adjacent eccentric, tapering soft-tissue mass corresponding to the noncalcified portion of a pelvic vein abutting a phlebolith) of whole stone and phlebolith were investigated. To investigate the presence of central lucency, soft tissue rim sign and comet-tail sign on stones and phleboliths, magnified images with x2 zoom factor were used. Bone window (350 HU/1300 HU) settings were used to see central lucency in addition to soft tissue window settings (45 HU/450 HU). Profile analysis which is a graphic representation of attenuation in each pixel along a line drawn through each calcification was performed. With this analysis, presence of central lucency in calcification (was seen as bifid peak at profile analysis) or uniform attenuation (was seen as single peak at analysis) were evaluated objectively. We also measured size and densities of stones and phleboliths. On the calcification area, 200 pixels were measured with using 10x20 pixel area. The lowest, highest and mean densities were recorded. In addition to density measurements, maximum transvers and vertical size of stones and phleboliths were measured. Window level and width for density and size measurement were 350 and 1300 respectively. Two radiologists independently interpreted the CT images and discrepancies were resolved by consensus. All measurements and assesments were done for two times and first measurements were used in the study since there was no statistically difference between two measurements. Mann - Whitney U test was used for comparing the size and density values of distal urinary stones and pelvic phleboliths. Chi-square test was used to compare central lucency, profile analysis, soft tissue rim sign and comet tail sign between two groups. Statistical significance was regarded as P less than 0.05. |
|||||||||||||||
| Results | |||||||||||||||
Mean diameters of stones detected on CT were measured as 6,4/6,0 mm (vertical/transvers) and ranged between (3,1-10,0/3,7-9,5). Mean diameters of phleboliths were 3,5 / 3,5 mm (vertical / transvers) and ranged between 1,5-7,5/1,5-7,1. This difference was significant statistically (p<0,05) (Table 1).
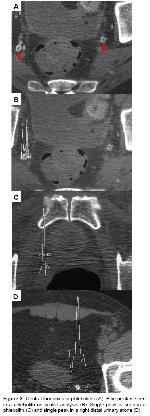
Fifty two of 80 phleboliths were round (65%) and 28 (35%) were oval shape. On the contrary, ten (32%) of 31 stone were round (Figure 1A), 8 (26%) of them were of oval shape. Geometric configuration was seen in thirteen (42%) stones (Figure 1B) but not in any phleboliths (Table 2). For urinary stones, the positive predictive value of a geometric shape was 100%.
Mean densities of phleboliths and stones were 386,5 HU (131 HU/935 HU) and 1088 HU (526 - 1594) (Figure 2), respectively (Table 1). This difference was statistically significant (p<0,05). Although 62 (78%) of 80 phleboliths had density value lower than 524 HU, all stones had density values more than 524 HU.
Eighteen (23%) of 80 phleboliths had central lucency (Figure 3A) and bifid peak (two peaks of high attenuation spanning a central region of lower attenuation) on profile analysis (Figure 3B). Sixty two (77%) phleboliths showed single peak on profile analysis (Figure 3C). There was neither subjective nor objective evidence at unenhanced helical CT of central low attenuation in any of the 31 stone, all of which had a single peak at profile analysis (Figure 3D). The difference between stones and phleboliths regarding central lucency and bifid peak on profile analysis was statistically significant. For phleboliths, the positive predictive value of both a central lucency and bifid peak at profile analysis was 100% (Table 3).
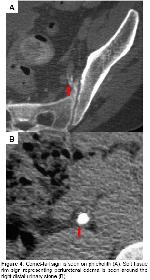
Although comet-tail sign was seen at 12 (15%) of 80 phleboliths (Figure 4A), we did not observe this sign at stones. We observed soft tissue rim sign on 21 (67%) of 31 stones (Figure 4B). However this sign was never seen on phleboliths (Table 3). These differences were statistically significant.
Resultantly, independent variables that correlated best with the diagnosis of a phlebolith were a central lucency, a bifid peak at profile analysis, and the comet-tail sign. Independent variables that correlated best with the diagnosis of a calculus were geometric shape, a single peak at profile analysis, the soft tissue rim sign, and mean attenuation greater than 524 HU. |
|||||||||||||||
| Discussion | |||||||||||||||
Unenhanced helical computed tomography (UHCT) has gained wide acceptance in the diagnosis of ureterolithiasis. CT has been reported to have 97% sensitivity, 96% specificity and 97% PPV in diagnosis of urinary stones2,3. A limitation of unenhanced helical CT in the evaluation of ureteral stone disease is difficulty in differentiating distal calculi from phleboliths since the critical localization and similar imaging findings of phleboliths4. This is a particular problem in middle-aged and elderly patients, who have a higher frequency of phleboliths; in thin patients, in whom a paucity of retroperitoneal and pelvic fat limits visualization of the distal ureter; and in patients with nonobstructing or partially obstructing ureter stones5. Similarly, secondary signs of urinary obstruction are not reliable all times because these findings could be found in patients who recently passed stone or stone causing partial or low-grade obstruction6. Since unenhanced CT has become the popular imaging technique in the evaluation of urinary stones, it is important to differentiate these two entities with objective criteria on unenhanced CT. According to literature shape, central lucency, density measurements, soft tissue rim sign, comet tail sign and profile analysis are all recommended for differentiation of phleboliths and urinary stones4,6,7,8. In this study, we assessed the efficacies of these criteria in differentiation. In our study, 35% of phlebolithis were oval, 65% were round. None of them were geometric. However 32% of stones were round, 26% were oval and 42% were geometric. The sensitivity, specificity and PPV of geometric shape for stones were 42%, 100% and 100%, respectively. These results indicates that shape feature can be used for differentiation of stones from phleboliths. Especially, geometric shape with its high specificity and high PPV, may strongly suggest the possibility of stone and enhances diagnosis in the pelvic calcifications (Figure 1B). Another criteria investigated in this study was density. We think that standardisation is critical in the measurement of densities. Centralization of calcification and exclusion of soft tissues from measurement area must be carefully applied (Figure 2). In our study mean densities of phleboliths and stones were significantly different from each other. However, these results differ from other studies in literature. In their study Bell et al. measured the mean density of phleboliths and stones as 160 HU (80 -278 HU) and 305 HU (221 – 530 HU) respectively4. The difference between these results may be attributed to different composition of stones and phleboliths in Turkish people. Although different density levels for stones and phleboliths are reported in literature, we think that mean density value is an objective criteria in distinction since it is a quantitative data. According to the measurements, densities of 62 (78%) of 80 phleboliths were under 524 HU, and density values of all stones were over 524 HU. The density values under 524 HU had 100% specificity and PPV for phleboliths in our study. Thus, our findings suggest density measurement as a reliable indicator for differentiation between stones and phleboliths. A central lucency in a calcification can be seen ideally in a magnified bone window (500 HU/2000 HU) images (Figure 3A). In vitro studies state that phleboliths tends to be round and contain central lucency, that calculi have opposite tendencies9. None of stones showed central lucency in our study. Although central lucency seems to be a specific indicator for phleboliths with its high specificity (100%) and PPV (100%) for phleboliths in our study reports in the literature stated that this finding could be shown in stones too7,10. We think that making profile analysis and showing bifid peak in this analysis is a more objective method for depicting low density in the central part of calcification than subjective visual assesment of central lucency. In our study, 23% of phleboliths showed central lucency and bifid peak on profile analysis (Figure 3B). In other studies, Fox et al. and Traubici et al. reported that these findings are not useful for stone-phleboliths differentiation. However Bell et al. suggested that these criteria may be helpful in differential diagnosis4,7,10. In our opinion, appropriate window setup and profile analysis facilitate the availability of these findings for this purpose. Comet-tail sign, a linear or curvilinear soft-tissue structure extending from an abdominal or pelvic calcification, generally indicates that a calcification is a phlebolith4,11. We found comet-tail sign in 15% of phleboliths, but not in any of the stones (Figure 4A). High specificity (100%) and PPV (100%) of this sign for phleboliths indicates its value in the distinction between phleboliths and urinary stones. The sensitivity of central lucency and bifid peak on profile analysis (23%) and comet-tail sign (15%) is low in the differentiation of distal urinary stones and phleboliths. Pre-sence of these criteria is significant in the distinction because their presence refers only phleboliths with their 100% value of specificity for phleboliths but has limited value because of low incidence. Soft tissue rim sign was found in 67% of stones and none of phleboliths. The specificity and PPV of this sign for stones are 100%. Also high NPV (86%) of this sign for urinary stones indicates its reliability. However Heneghan et al. and Bell et al. found this sign in 8% and 2% of phleboliths4,6. The difference of these studies from our study in this subject may be according to CT technique. We used 2 mm section thickness and 2 mm gap that would prevent misdiagnosis of noncalcified portion of pelvic vein as soft tissue rim sign (Figure 4B). The results of this study indicate that unenhanced helical CT has reliable findings in the differentiation of stones from phleboliths. Presence of central lucency, bifid peak on profile analysis and comet tail sign have 100% specificity and PPV for diagnosis of phleboliths. These findings are not seen usually (23%, 23% and 15% respectively) but presence of them in a calcification means no possibility for stone. Geometric shape and soft tissue rim sign have high sensitivity and specificity values for stone detection. Differences in density values of stones and phleboliths are reliable and distinctive criteria for this purpose. It is easier to differentiate urinary stones from phleboliths with thin-slice CT. Applying of all criteria mentioned in this study may be useful in differentiation of distal urinary stones from phleboliths on unenhanced helical CT. The results of this study indicate that unenhanced helical CT has reliable findings in the differentiation of stones from phleboliths. It is easier to differentiate urinary stones from phleboliths with thin-slice CT. Applying of all criteria mentioned in this study may be useful in differentiation of distal urinary stones from phleboliths on unenhanced helical CT. |
|||||||||||||||
| References | |||||||||||||||
1) Vieweg J, Teh C, Freed K, Leder RA, Smith RHA, Nelson RH, Preminger GM. Unenhanced helical computerized tomography for the evaluation of patients with acute flank pain. J Urol 1998; 160: 679-684.
2) Katz DS, Lane MJ, Sommer FG. Unenhanced helical CT of ureteral stones: incidence of associated urinary tract findings. AJR Am J Roentgenol 1996; 166: 1319-1322.
3) Smith RC, Levine C, Rosenfeld A. Helical CT of urinary stones: Epidemiology, origin, pathophysiology, diagnosis, and management. Radiol Clin North Am 1999; 37: 911-952.
4) Bell TV, Fenlon HM, Davison BD, Ahari HK, Hussain S. Unenhanced helical CT criteria to differentiate distal ureteral calculi from pelvic phleboliths. Radiology 1998; 207: 363-367.
5) Fielding JR, Steele G, Fox LA, Heller H, Loughlin KR. Spiral computerized tomography in the evaluation of acute flank pain: a replacement for excretory urography. J of Urol 1997; 157: 2071-2073.
6) Heneghan JP, Dalrymple NC, Verga M, Rosenfield AT, Smith RC. Soft-tissue ‘rim' sign in the diagnosis of ureteral calculi with use of unenhanced helical CT. Radiology 1997; 202: 709-711.
7) Traubici J, Neitlich JD, Smith RC: Distinguishing pelvic phleboliths from distal ureteral stones on routine unenhanced helical CT. Is there a radiolucent center? AJR 1999; 172: 13-17.
8) Arac M, Celik H, Oner AY, Gultekin S, Gumus T, Kosar S. Distinguishing pelvic phleboliths from distal ureteral calculi: thin-slice CT findings. Eur Radiol 2005; 15: 65-70.
9) Mindell HJ, Herschorn SD, Dash A, et al. In vitro CT comparisons of dissected phleboliths and retrieved ureteral calculi. Emergency Radiology 2001; 8: 332-334.
|
|||||||||||||||
| [ Başa Dön ] [ Özet ] [ PDF ] [ Benzer Makaleler ] [ Yazara E-Posta ] [ Editöre E-Posta ] | |||||||||||||||
| [ Ana Sayfa | Editörler | Danışma Kurulu | Dergi Hakkında | İçindekiler | Arşiv | Yayın Arama | Yazarlara Bilgi | E-Posta ] |